
Nurse Alters Morphine Record, Patient Dies: CNO Orders Permanent Resignation
A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

The only thing worse than a diagnosis of cancer is discovering your cancer diagnosis was missed and treatment was delayed. For some, this could mean the difference between life and death. This post explores some of the common causes of cancer misdiagnosis in the medico-legal context as well as the specific evidentiary requirements to prove a cancer misdiagnosis lawsuit in Ontario.
COMMON CAUSES OF CANCER MISDIAGNOSIS
In a 2019 study by the American Society for Healthcare Risk Management of the American Hospital Association entitled “Missed diagnosis of cancer in primary care: Insights from malpractice claims data” the authors observed that in the ambulatory setting, missed cancer diagnoses are leading contributors to patient harm and malpractice risk.
The researchers in this study analyzed 2155 diagnostic error malpractice claims in outpatient general medicine.
The results were as follows: Missed cancer diagnoses represented 980 (46%) cases of primary care diagnostic errors, most commonly from lung, colorectal, prostate, or breast cancer. The majority (76%) involved errors in clinical judgment, such as a failure or delay in ordering a diagnostic test (51%) or failure or delay in obtaining a consult or referral (37%). These factors were independently associated with higher-severity patient harm. The majority of these errors were of high severity (85%).
The authors of this study concluded that malpractice claims involving missed diagnoses of cancer in primary care most often involve routine screening examinations or delays in testing or referral.
In my experience as a medical malpractice lawyer practicing primarily in the Greater Toronto Area, I have found the following to be the most common causes of cancer misdiagnosis:
Any error and corresponding delay in the diagnosis of cancer can be serious. Since medical malpractice claims are about compensation, an essential element of succeeding in a cancer malpractice claim is proving that the delay in treatment caused harm.
HOW DO I PROVE A MISDIAGNOSIS OF CANCER CLAIM?
Proving any kind of medical malpractice claim in Ontario is challenging. For a detailed overview on whether you can sue for medical malpractice, please read this post.
A misdiagnosis of cancer claim has a particular set of obstacles that will need to be overcome in order to result in compensation to the victim of malpractice and their family. Sadly, most delayed diagnosis claims are brought by the estate of the patient as the delay in cancer diagnosis will have resulted in a late stage diagnosis with a fatal end.
Expert evidence is required to prove virtually all medical malpractice claims. In a delayed or missed diagnosis of cancer claim, you will first have to prove that a physician, hospital, nurse or other health care professional fell below the standard of care of a reasonable and careful professional in similar circumstances.
With respect to communication errors, this is often fairly straightforward as preliminary investigations will often reveal the nature and source of the communication breakdown. Proving investigative errors will require expert consultation in the appropriate field as there are often standards of practice with respect to cancer screening and surveillance as well as indications (and contra-indications) for certain cancer tests based of patient demographics and presenting complaints. Interpretation errors will similarly require input of a properly qualified expert to fairly and objectively interpret radiological images or pathological specimens to ensure reasonable care and expertise was employed in interpreting and reporting on the investigation at issue.
More often than not the most contentious issue will be causation. This is a legal requirement to succeed in a medical malpractice claim. You must prove that the substandard care caused harm. Every case is different.
For starters, there is a wide range of types of cancer, the most common being:
Cancers are further categorized by grade and stage.
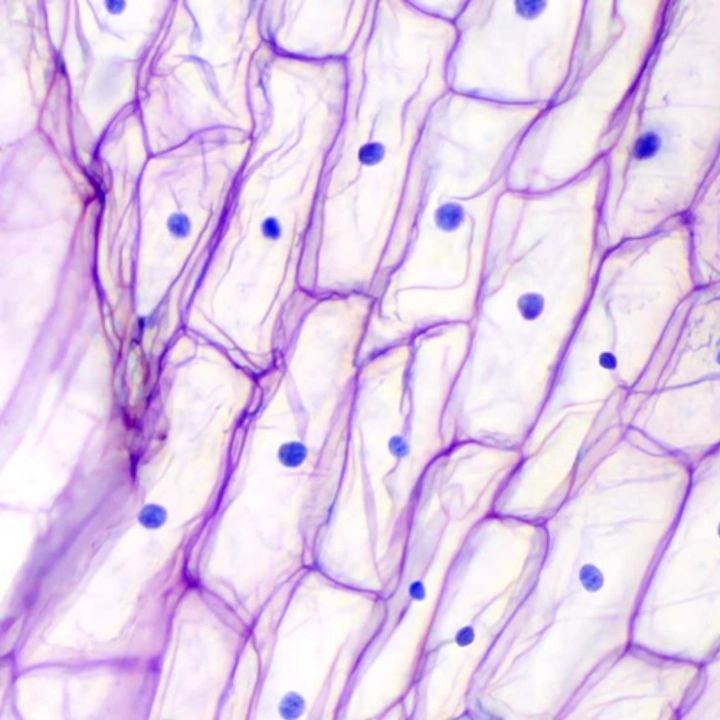
Cancer grade is based on how the cancer cells look. The cancer grade will predict how fast the cancer will grow and how likely it is to spread. Grade is usually described using a number from 1 to 3 or 4. The higher the number, the more different the cancer cells look from healthy cells and the faster they are growing.
Cancer stage relates to how much cancer is in your body, where it is and how far it has spread. Cancer can spread within the organ that it started in, to nearby lymph nodes or to distant sites. Stage is described using a number from 1 to 4. Stage 1 cancer is usually small and has not spread outside of where it started. The higher the number, the larger the tumour or the more it has spread. Stage 4 usually means it has spread to distant sites.
The Canadian Cancer Society website is a great resource for more more information about cancer grades and stages.
Treatment options and prognosis will vary depending on type, grade and stage of cancer. In order to prove causation in a medication malpractice claim you will need opinion evidence from an oncologist on what the likely grade and stage of the misdiagnosed cancer would have been at the time it should have been diagnosed. You will further need to prove that available treatment at the time the cancer should have been diagnosed would likely have improved the patient’s outcome.
It should be no big surprise that these claims are invariably defended on the basis that earlier diagnosis and treatment would still have resulted in the death of the patient. Depending on the type, grade and stage of cancer, and the duration of the delay in diagnosis, this may be true. Generally the longer the delay in diagnosis, the more likely that earlier intervention would have improved outcome.
Although proving a delayed diagnosis medical malpractice claim is challenging, it is not impossible. If you are concerned that you or a loved one’s cancer diagnosis was delayed, you should seek legal advice.

A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

What College of Physicians and Surgeons of Ontario v. Thirlwell, 2026 ONPSDT 5 Means for Patients and Public Trust In College of Physicians and Surgeons