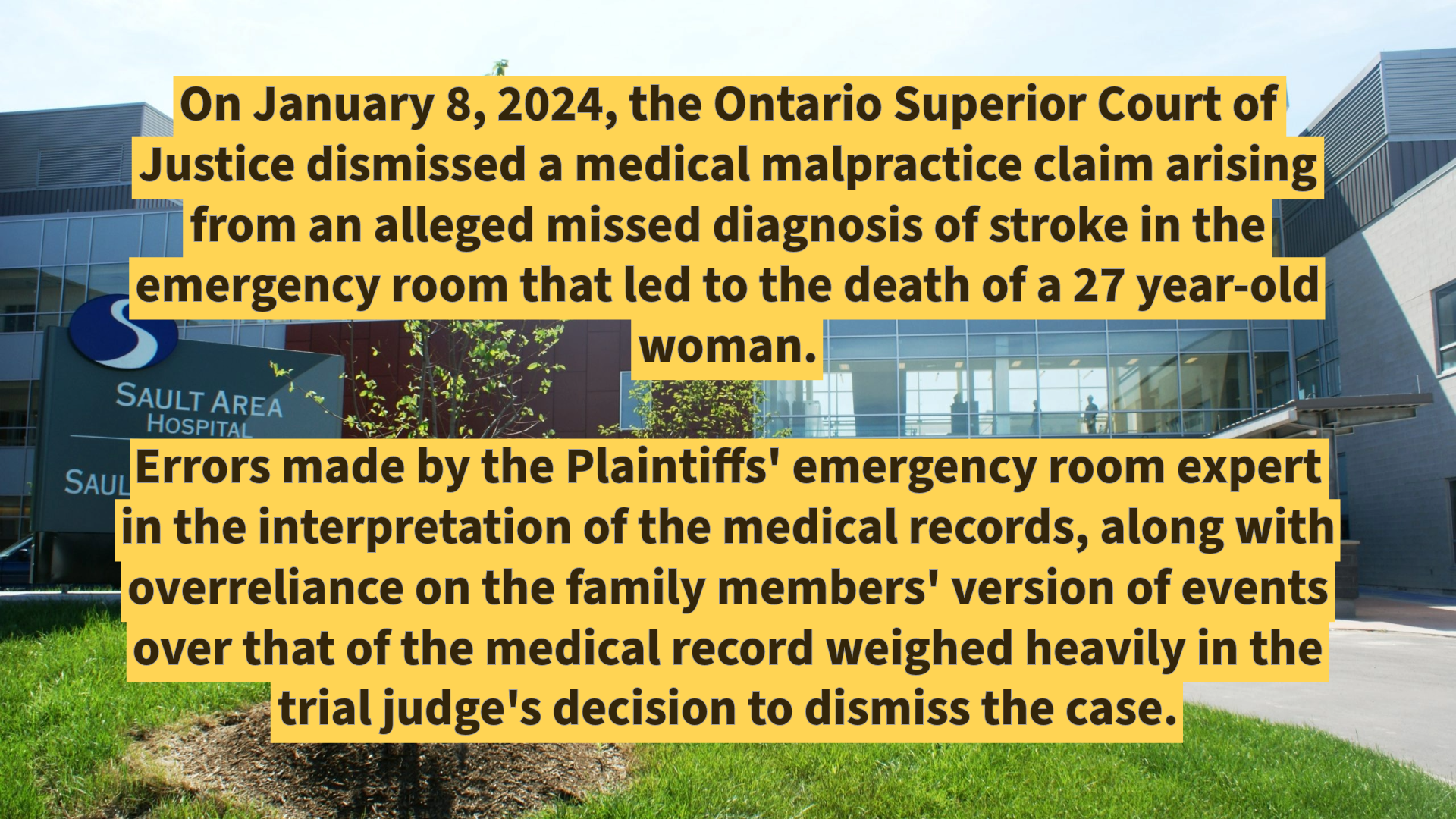
On January 8, 2024, the Ontario Superior Court of Justice dismissed a medical malpractice claim arising from an alleged missed diagnosis of stroke in the emergency room that led to the death of a 27 year-old woman.
Errors made by the Plaintiffs’ emergency room expert in the interpretation of the medical records, along with overreliance on the family members’ version of events over that of the medical record weighed heavily in the trial judge’s decision to dismiss the case.
FACTS
The Plaintiff, Philisha Sutherland (“Philisha”) was a 27 year-old woman who resided with her parents, Donna and Earle Sutherland.
On October 17, 2013, Philisha’s father returned from work and he found Philisha to be unwell. When the mother arrived home from work a short time after her husband, a decision was made to call 911 and an ambulance was dispatched which ultimately transported Philisha to the Sault Area Hospital.
While she was a patient at the Sault Area Hospital, Philisha was treated by the Defendant emergency medicine physician, Dr. Karen Booth.
A course of treatment was followed for Philisha under the supervision and direction of Dr. Booth. Philisha was discharged that evening from the hospital and went straight to bed at home.
The next morning, on October 18, 2013, the parents checked on Philisha who said she was feeling fine and did not require her parents at home to provide care for her. The parents went to work and when they came home in the late afternoon they discovered Philisha at home in a bad state. Philisha was in a significantly worse condition than she was when they left her to go to work in the morning. The interior of the home was ransacked with items of furniture overturned and closet doors off the hinges. Philisha had injuries to her body, including cuts, bruises, and a large goose egg type bruise on her forehead.
An ambulance was dispatched and Philisha was transported to the Sault Area Hospital. Upon arrival at the hospital it was determined that Philisha had severe brain swelling compressing her brain stem and that she had suffered cerebellar infarct primarily involving a medial component of the left cerebellum. Philisha was brain dead. She was kept on life support until October 21, 2013 at which time life support was discontinued and Philisha was pronounced dead.
The Plaintiffs asserted through their expert in emergency medicine that Dr. Booth fell below the standard of care of an emergency room physician in managing Philisha’s emergency department attendance of October 17, 2013 for the following five reasons:
- She failed to investigate the significantly elevated white blood cell count of 31, 600;
- She incorrectly concluded the patient’s presentation on October 17, 2013 was consistent with marijuana intoxication;
- She failed to perform a thorough and acceptable neurological examination because she did not carry out a gait assessment;
- She failed to consider any other differential diagnosis to explain the patient’s clinical presentation on October 17, 2013; and
- That given this patient’s clinical presentation of neurological symptoms, she failed to request a non-contrast CT scan of the patient’s head.
DECISION
Standard of Care
Upon hearing the evidence of the family, the treating health care professionals and the expert witnesses, the trial judge arrived at the conclusion that the Plaintiffs had failed to prove that Dr. Booth fell below the standard of care in her treatment of this patient.
Moreover, the trial judge was thoroughly unimpressed with the opinion of the Plaintiffs’ expert in emergency medicine noting multiple errors and misinterpretations of the evidence (at paras. 139-140):
I was not impressed by what was left of Dr. Brankston’s opinion after cross-examination was completed. It is fair to state that Dr. Brankston’s report and opinion was unravelled to a great extent during cross-examination and the court was left with no confidence in the conclusions reached by Dr. Brankston or his opinion that Dr. Karen Booth did not meet the standard of care expected by an emergency room physician on October 17, 2013.
If the only evidence the court had was the evidence of Dr. Brankston on the standard of care, the court would conclude that there was no evidence of a breach of the standard of care that the court could rely on in this case and the action would have to be dismissed.
Causation
On the issue of causation, the difference of opinion between the neurologists was the timing of the stroke. Essentially, the Plaintiffs’ position was that the patient was suffering from a stroke on October 17, 2013 and the emergency medicine physician missed it. The defence position was that the patient actually suffered a stroke the next day such that could not have been diagnosed earlier.
In preferring the defence expert’s opinion, the trial judge noted that the Plaintiffs’ neurologist relied heavily on the subjective reporting of the patient’s family that was not corroborated in the medical records. The defence expert relied only on the medical records. The trial judge observed [at para. 164]:
If I had to make a choice, I would prefer an opinion based on the medical documentation and how Philisha Sutherland presented at the Sault Area Hospital over an opinion which relied on information from collateral sources, some of which has proved to be inaccurate and all of it is not supported by what the health care professionals observed in their interactions with Philisha Sutherland at the Sault Area Hospital.
Damages
Had the Plaintiffs been successful (which they were not), the trial judge would have awarded damages for the death of a 27 year-old woman with no dependents as follows:
- $75,000 for each of the parents.
- $40,000 for the adult sibling.
- $20,000 for the grandfather (who died before the trial).
EXPERT LIABILITY WITNESSES
Plaintiffs’ Experts
Dr. Edwin Brankston was qualified as an expert on the standard of care of an emergency physician in 2013.
Dr. Brankston graduated from the medical school at Queen’s University in 1976. Dr. Brankston is qualified by the College of Family Physicians with a specialty in family medicine and emergency medicine. Dr. Brankston entered practice in 1977 and worked primarily at the Oshawa Hospital. Dr. Brankston has prepared opinions and chart audits for the College of Physicians and Surgeons in Ontario involving standards of care for physicians. From 1977 to 1996, Dr. Brankston worked part-time in the Oshawa General Hospital as an emergency physician, working one or two shifts a week. From 1995 to 2007, Dr. Brankston took a 12-year hiatus from practicing emergency room medicine. He resumed his emergency room practice in 2007, working one or two shifts each week until his retirement in 2018.
Dr. Bryan Young was qualified as an expert in neurology and gave causation evidence with respect to the patient’s stroke.
Defence Experts
Dr. Marco Sivilotti was qualified as an expert on the issue of the standard of care expected of an emergency room physician.
Dr. Sivilotti graduated from medical school at Queen’s University in 1988. He received his specialty in emergency medicine in 1994 and is U.S. board certified in emergency medicine and a fellow of the American College of Emergency Physicians since 1998. Dr. Sivilotti is a practicing emergency physician and is a full professor emergency medicine at Queen’s University in Kingston, Ontario. Dr. Sivilotti also completed training in medical toxicology at the University of Massachusetts, and since 2014, has been a fellow of the American College of Medical Toxicology. Dr. Sivilotti’s professional experience is in emergency medicine and medical toxicology.
Dr. Sivilotti was not permitted to provide an opinion on the timing of the stroke suffered by the patient as it was determined to be outside his expertise as an emergency medicine physician.
Dr. David Spence was qualified as an expert in neurology and was permitted to provide an opinion causation as it related to the patient’s stroke.
Decision Date: January 8, 2024
Jurisdiction: Ontario Superior Court of Justice
Citation: Sutherland et al. v. Booth, 2024 ONSC 127 (CanLII)