
Nurse Alters Morphine Record, Patient Dies: CNO Orders Permanent Resignation
A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one
Cauda equina syndrome (CES) is the compression of a collection of nerve roots called the cauda equina. CES is a recognized surgical emergency and may require emergent spinal surgery. As such, delayed diagnosis and treatment of CES is a common medical-legal concern for physicians, nurses and hospitals.
WHAT IS CES?
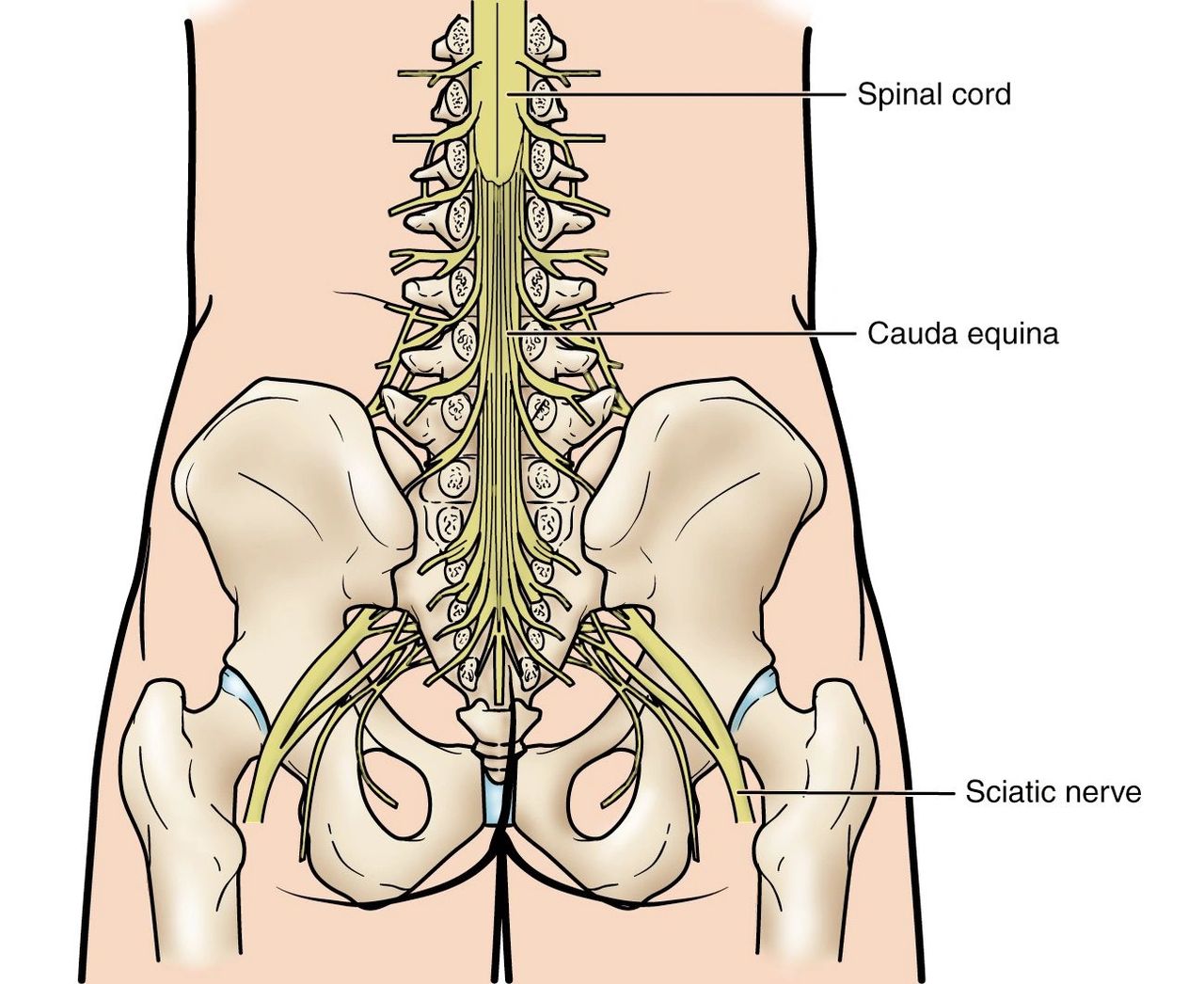
The cauda equina is a collection of nerve roots shaped like a horse’s tail. It is located at the bottom of your spinal cord.
The cauda equina nerves allow you to move and feel sensations in your legs and urinary bladder. Compressed cauda equina nerves can cause pain, weakness, incontinence and other symptoms. This syndrome can cause permanent damage, including paralysis, if left untreated.
According to the American Association of Neurological Surgeons, potential causes of CES include:
CES may present with a range of symptoms, the severity of which depends on the degree of compression and the precise nerve roots that are being compressed.
Patients with CES may experience some or all of these “red flag” symptoms:
If a patient is experiencing any of the “red flag” symptoms above, immediate medical attention is required to evaluate whether these symptoms represent CES.
Once the diagnosis of CES is made and the etiology established, urgent/emergent surgery is usually the treatment of choice. The goal is to free up the compressed nerve roots to improve the likelihood of recovery. Left untreated, CES can result in permanent paralysis and incontinence.
CES AND MEDICAL MALPRACTICE
As with all medical malpractice claims, the two most important legal issues that the patient must prove in order to succeed is a breach of the standard of care and causation.
With respect to standard of care, delayed diagnosis of CES may occur at the primary care level with family or emergency medicine physicians missing signs and symptoms of this condition. It may also happen in hospital under the care of nurses while a patient is recovering from orthopedic or neurosurgery. Given that not all hospitals have surgical services equipped to treat CES, delay can sometimes arise in transferring patients to appropriate centers for definitive treatment.
There may also be situations where investigations are ordered but are not properly interpreted or reported by a radiologist.
Causation is the other and most often more contentious legal issue in CES medical malpractice claims. In a medical malpractice lawsuit the patient has the burden of proving that the negligence care caused harm. If it cannot be proven that harm was caused by the substandard care, then the patient will lose their lawsuit.
With respect to CES, there is no scientific guarantee that by relieving the compression on the cauda equina that the nerve roots will fully regenerate and heal. That being said, it is generally recognized that the earlier this surgery takes please, the better the likely outcome will be for the patient.
For instance, in an article published in the American Journal of Medicine entitled “Evaluation and Management of Cauda Equina Syndrome” the authors observe that: Once suspected, emergent spinal surgery referral is indicated, along with urgent decompression. Even with expeditious surgery, improvements remain inconsistent. However, early intervention has been shown to portend greater chance of neurologic recovery. All providers in clinical practice must understand the severity of this condition. Providers can optimize long-term patient outcomes and minimize the risk of litigation by open communication, good clinical practice, thorough documentation, and expeditious care.
Every case is different, but certainly the longer the delay in treatment, the stronger the argument will be that earlier surgery would have likely improved the outcome for patients who are left with residual morbidity, such as paralysis and/or incontinence, following CES.

A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

What College of Physicians and Surgeons of Ontario v. Thirlwell, 2026 ONPSDT 5 Means for Patients and Public Trust In College of Physicians and Surgeons