
Nurse Alters Morphine Record, Patient Dies: CNO Orders Permanent Resignation
A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one
On January 13, 2025, Justice Robert Centa of the Superior Court of Justice of Ontario dismissed a medical malpractice claim by the family of 56 year-old patient who died of an aortic dissection.
The family had alleged negligence on the part of an internal medicine physician who had seen the patient 3 years earlier who they alleged should have conducted more tests and followed the patient more closely which they argued would have led to the identification and treatment of the aortic concerns prior to the fatal dissection.
The family also alleged negligence as against an emergency medicine physician that the patient had seen about 2 months before his death with complaints of chest pain in the setting of hypertension. Based on reassuring investigations and medical management of the hypertension in the emergency room, the patient was discharged to follow up with his family physician.
The trial judge found that these physicians met the standard of care. The claim was dismissed.
On November 5, 2012, Mr. McMullan initially visited a walk-in clinic feeling unwell. He was diagnosed with high blood pressure and an irregular heartbeat. He was sent to the emergency department at the Leamington Hospital where Dr. Sarfraz prescribed metoprolol and referred him to Dr. Naom for a consultation.
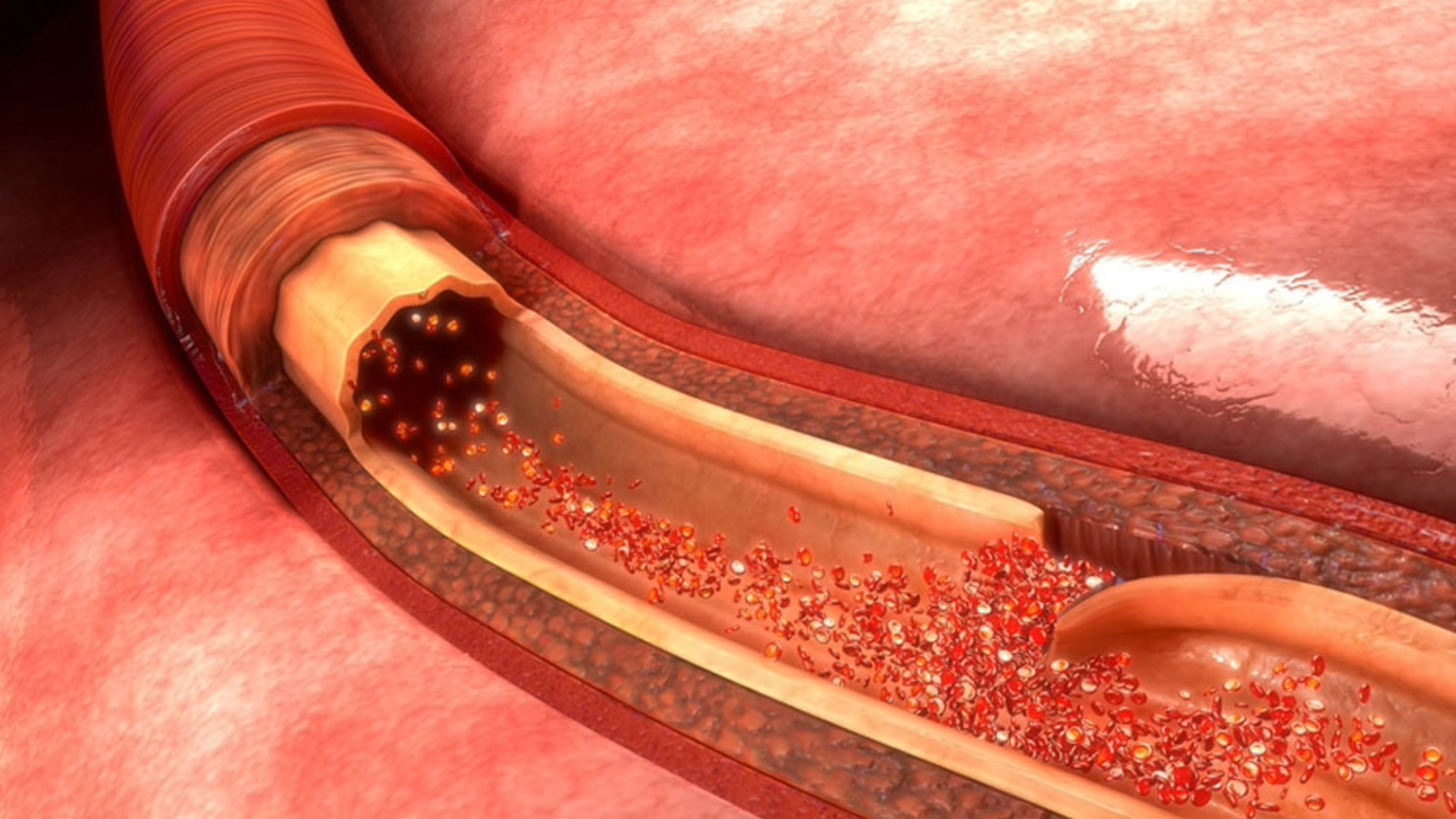
Mr. McMullan underwent an echocardiogram test on November 28, 2012. The test indicated mild aortic root dilation. Dr. Naom provided a detailed interpretation of the test results, which included atrial fibrillation, tricuspid regurgitation, elevated right ventricular systolic pressure, and mild concentric left ventricular hypertrophy.
Dr. Naom consulted with Mr. McMullan again on December 13, 2012. Despite the test results, Mr. McMullan reported no symptoms such as chest pain, shortness of breath, or palpitations. Due to a skin rash, Dr. Naom switched Mr. McMullan’s prescription from ramipril to losartan and explained that the aortic dilation was not clinically significant.
During a follow-up consultation on January 24, 2013, Dr. Naom noted that Mr. McMullan was only taking metoprolol once a day instead of the prescribed twice a day and stressed the importance of adhering to the medication routine.
On February 25, 2013, Mr. McMullan’s blood pressure and heart rate were within the target range, and he reported feeling well.
In his final consultation on May 28, 2013, Mr. McMullan was stable, with well-controlled blood pressure and no health complaints. Dr. Naom sent a sign-off letter to Dr. Blanchard and handed over Mr. McMullan’s care back to his family physician.
Years later, on February 29, 2016, Mr. McMullan attended the emergency department at Leamington Hospital and saw Dr. El Jaoudi. He had high blood pressure and symptoms of chest pain. An initial assessment was performed at 2350h, and tests including a complete blood count, glucose test, electrocardiogram, and chest x-ray were ordered. All test results were found to be normal, effectively ruling out acute pathology and end organ damage. Dr. El Jaoudi proceeded to prescribe labetalol to manage Mr. McMullan’s high blood pressure. At 0200h, a reassessment revealed that the patient’s blood pressure was well controlled. Ultimately, Dr. El Jaoudi made the clinical decision to discharge Mr. McMullan on the condition he follow up with his family physician within one week.
Unfortunately, on May 3, 2016, Mr. McMullan suffered a 1.5 cm tear in his aorta which caused his sudden and unexpected death. Mr. McMullan was 56 years old.
Standard of care and causation with respect to the defendant physicians were at issue in this trial. Damages were settled prior to trial at $596,500 inclusive of any and all taxes, pre-judgment interest, and subrogated claims.
Dr. Dave Nagpal was qualified as an expert in cardiac surgery, including the assessment, diagnosis, management, and treatment of aortic dilatations and aortic dissections, to provide opinion evidence on surgical assessment, management, decision making, and treatment of Mr. McMullan and the probable outcome of that surgery had it occurred.
Dr. Alan Drummond was qualified as an as an expert emergency department physician qualified to provide opinion evidence on the standard of care expected of an emergency department physician on February 29, 2016, including the diagnosis, assessment, and management of patients presenting to the emergency department with chest pain and hypertension, and hypertensive crisis.
Dr. Mirek Otremba was qualified as an internal medicine specialist to provide opinion evidence at trial regarding:
Dr. Ian Preyra was qualified as an expert in emergency medicine and post-mortem examinations, qualified to give opinion evidence on the standard of care expected of an emergency department physician on February 29, 2016, the interpretation of the post-mortem examination of May 17, 2016, and the foreseeability of Mr. McMullen’s aortic dissection on May 3, 2016
Dr. Sandeep Kohli was qualified as an expert in internal medicine to provide opinion evidence on the standard of care expected of an internal medicine specialist in 2012 and 2013, and on whether the internal medicine care provided by Dr. Naom caused or contributed to Mr. McMullen’s death on May 3, 2016
Dr. Gideon Cohen was qualified Dr. Cohen as an expert cardiac surgeon qualified to provide opinion evidence on the assessment, diagnosis, management, and treatment of aortic dilatations and aortic dissection, and whether further imaging on or after November 28, 2012, would have prevented Mr. McMullen’s death on May 3, 2016.
After reviewing all the evidence, the court determined that Dr. Noam met the standard of care in his treatment of Mr. McMullan. This decision was based on several key factors.
Firstly, Dr. Naom’s interpretation of the echocardiogram and his decision not to recommend further imaging of Mr. McMullan’s aorta was deemed correct.
The court also reviewed Dr. Naom’s management of Mr. McMullan’s hypertension and cardiovascular risk factors, which was determined to meet the standard of care. Dr. Noam’s interpretation and management of the stress test and Persantine MIBI test were also found to meet the standard of care. The court supported Dr. Naom’s conclusion that Mr. McMullan’s aorta was normal, rejecting the plaintiffs’ purported evidence to the contrary.
Lastly, Dr. Noam’s recommendations for ongoing care were seen as reasonable, with no need for additional follow-up imaging or testing.
The trial judge found that Dr. El Jaoudi’s met the standard of care for Mr. McMullan for several reasons. Initially, no breaches were found in his approach, as there was no significant history of aortic dilatation to consider. Furthermore, Dr. El Jaoudi successfully ruled out end organ damage as the clinical findings were all reassuring.
The trial judge found that Dr. El Jaoudi’s decision not to perform a fundoscopy or order a urinalysis did not contravene the standard of care due to the challenging nature of these procedures and the lack of necessary indicators. The decisions not to order serial electrocardiogram or troponin testing were also in line with the standard of care, as the initial test results were reassuring and there were no indications of myocardial ischemia.
Additionally, it was found that Dr. El Jaoudi provided appropriate instructions for discharge and follow-up care to Mr. McMullan. With all clinical circumstances and reassuring test results in mind, his decision to discharge Mr. McMullan was reasonable and within standard practice.
Based on the above, the claim was dismissed as against the physicians.
Decision Date: January 13, 2025
Jurisdiction: Ontario Superior Court of Justice

A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

What College of Physicians and Surgeons of Ontario v. Thirlwell, 2026 ONPSDT 5 Means for Patients and Public Trust In College of Physicians and Surgeons

Estate of Henders v. Lakeridge Health Oshawa, 2026 ONSC 701 In a significant decision for medical malpractice and long-term care litigation in Ontario, the Superior

What CPSO v. Faruqi Means for Patients and Physicians On January 21, 2026, the Ontario Physicians and Surgeons Discipline Tribunal released an important decision addressing