
Nurse Alters Morphine Record, Patient Dies: CNO Orders Permanent Resignation
A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one
Toronto medical malpractice lawyers Paul Cahill and Hudson Chalmers successfully prosecuted a medical malpractice claim against a negligent emergency medicine physician who caused the death of a young married mother of four children. At the time of her death, the children were aged 7, 5, 4 and 2.

On September 6, 2023, the Honourable Mr. Justice William LeMay of the Ontario Superior Court of Justice found the Defendant emergency room physician, Dr. Jeffrey Handler (“Dr. Handler”) negligent in his care of the Plaintiff, Elisha Shaw (“Elisha”), which resulted in her death.
This medical malpractice lawsuit involved the management of a patient with a history of gastric bypass surgery who presented to the William Osler Health System – Brampton Civic Hospital emergency room with acute abdominal pain and had radiological findings suggestive of an internal hernia.
The emergency room physician discharged the patient home despite the fact that her abdominal pain remained uncontrolled throughout her visit and did not call her back to organize an urgent in-hospital consultation with a general surgeon after learning of the radiological findings.
The patient returned to the emergency room the next day by ambulance in a worse condition and ultimately died of complications associated with bowel ischemic and necrotic bowel.
The trial took place over 12 days in January, 2023 in Brampton, Ontario.
ISSUES
The following issues were in dispute at this trial:
FACTS
Elisha had a history of on and off abdominal pain for several years following bariatric surgery in 2012 for weight loss.
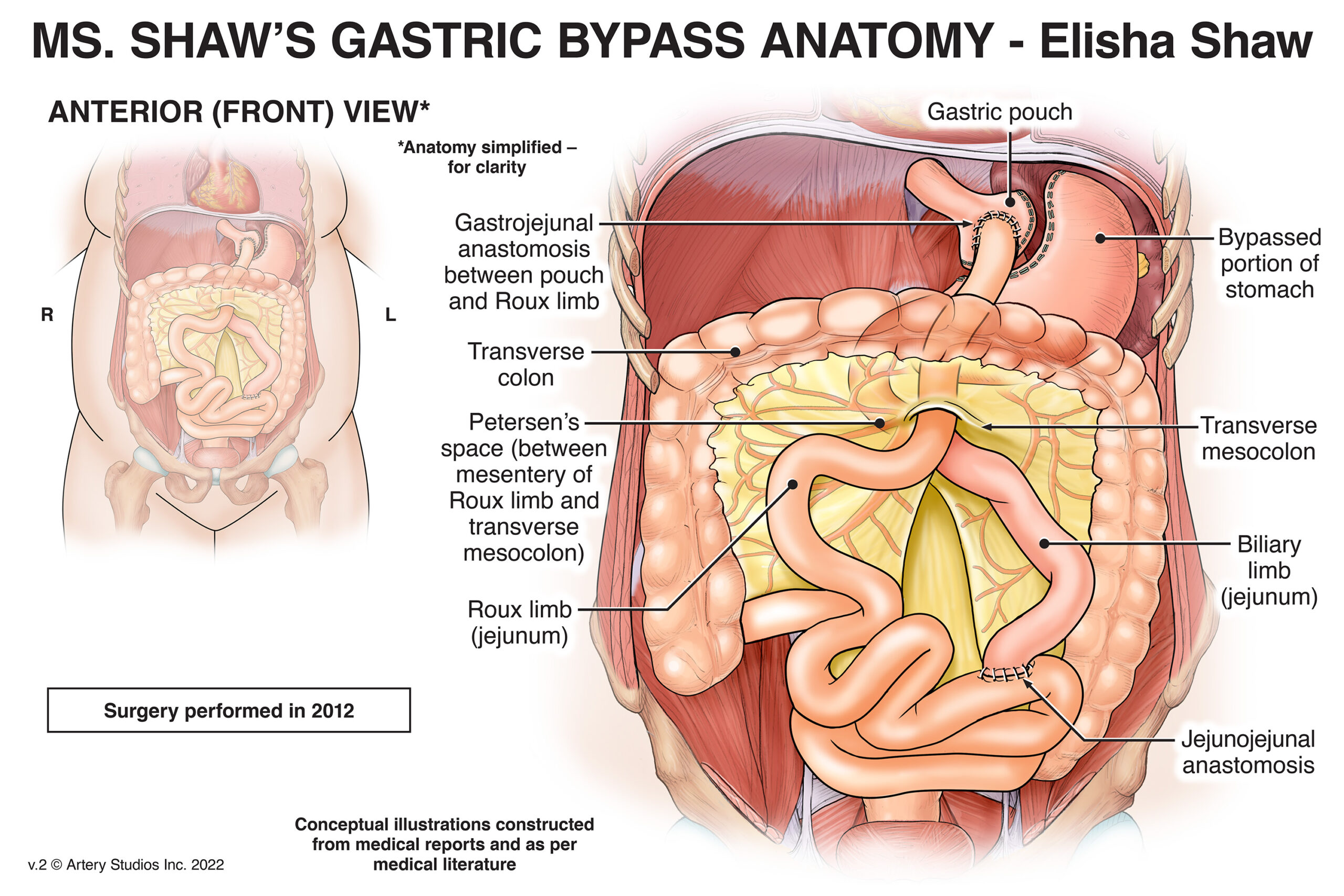
The bariatric surgery that was performed on Elisha was designed to reduce the size of the stomach and, as a result, the appetite and calorie consumption of the person upon whom the surgery was performed.
The result, as illustrated above, is that the patient will have fewer intestines in the abdominal cavity, which can cause them to move around and become tangled.
Years after the surgery, Elisha’s abdominal pain became intense that on the evening of November 16, 2015, she had her husband Merton take her to the emergency room of William Osler Health System – Brampton Civic Hospital.
She arrived at about 11:30 p.m. She had to be transported into the emergency room in a wheelchair. She had diffuse abdominal and back pain.
She was first seen by the nursing staff and then referred to Dr. Handler. When she was seen by the nursing staff, she was triaged and given a 2 on the Canadian Triage and Acuity Score (“CTAS”).
The CTAS score is a tool used to triage patients. A 2 on the CTAS scale means that the patient is in significant distress and should generally be seen by a physician within a half an hour of being admitted.
Dr. Handler was the emergency room physician on duty that was responsible for Elisha’s care during this visit.
The following is a detailed chronology of the events that followed.
November 16, 2015 – 11:38 p.m.
Elisha arrived at the hospital, was triaged, and her vital signs were taken. The vital signs were grossly normal. She arrived by wheelchair. Pain score 10/10.
November 17, 2015 – 12:10 a.m.
Dr. Handler conducted a physical exam on Elisha. Her abdomen was soft and there was no “rebound tenderness”, which would have been a physical sign of an underlying problem.
Dr. Handler also took a history from Ms. Shaw and reviewed the history that had been provided by the nurses.
12:20 a.m.
Dr. Handler ordered a series of blood tests, which were standard for abdominal pain and other tests.
Dr. Handler ordered a CT scan of Elisha’s bowel and abdomen to determine whether there was a bowel obstruction.
Dr. Handler ordered both an IV drip and pain medications, Gravol and morphine.
12:30 a.m.
Elisha was assessed and her vitals were taken again. Her blood pressure had changed, her complaints of pain had not changed (pain score 10/10), and the vitals were generally normal.
12:40 a.m.
Nursing staff return from break and were advised of the orders in respect of the IV and the medications. Elisha was to be sent for her CT Scan. Gravol and 6 mg of morphine were administered.
1:20 a.m.
Elisha continued to experience considerable pain, even after the administration of 6 mg of morphine. An additional 4 mg was ordered
2:24 a.m.
Abdominal CT imaging was performed
3:00 a.m.
Elisha returned from the Diagnostic Imaging department still complaining of significant pain. Vitals were taken and remained similar. Pain score remained 10/10
3:30 a.m.
Dr. Handler ordered 10 mg of Buscopan to be administered by IV.
3:40 a.m.
The Buscopan was administered. Elisha had to have a new IV started because she may have removed hers.
4:00 a.m.
Elisha and Merton both noted to be sleeping by the nursing staff. No breathing distress noted.
Dr. Handler discussed the CT scan with the overnight remote radiologist, Dr. Singer-Jordan. All that was noted by Dr. Singer-Jordan was the presence of ovarian cysts and nodes. No obstruction was noted.
4:45 a.m.
Elisha woke up and was crying aloud about the pain. Elisha was noted to be unmanageable and her husband, Merton, was demanding that she be given more pain medications. She was given 15 mg of Toradol.
5:02 a.m.
Elisha’s vitals are taken again. They had not significantly changed since admission.
5:10 a.m.
An elixir of KCL (which is a potassium supplement) was ordered for Elisha.
5:20 a.m.
Elisha was reassessed by the nursing staff and determined to still be having diffuse abdominal pain. The level of pain had not changed and remained 10/10.
5:36 a.m.
The KCL was administered to Elisha. She was still crying and demanding more pain medications.
5:47 a.m.
Merton left to go for a walk outside. Elisha was still in pain at this point and was still demanding more morphine.
6:40 a.m.
Elisha was “still the same” according to the nursing staff.
7:00 a.m.- 7:15 a.m.
Dr. Handler assessed Elisha and discharged her home with a prescription for Buscopan. The nursing notes reflected that Elisha did not disagree with the decision to discharge her home.
Dr. Handler testified at trial that Elisha’s pain had decreased and that he made a note of that on the emergency record. The nursing notes did not have any indication of a change in Elisha’s pain presentation.
By 8:00 a.m.
The staff radiologist Dr. Fitzgerald reviewed the CT scan from the night before and determined that there was twisting of the mesenteric vessels, which could suggest a bowel obstruction. She communicated those findings (which are different from the findings of Dr. Singer-Jordan) to Dr. Handler.
Dr. Fitzgerald testified at trial as a participant expert. Her testimony, which was accepted by the trial judge, was that she contacted Dr. Handler in the morning of November 17, 2015 for two reasons.
For his part, Dr. Handler testified that he did not recall the details of this conversation although he did provide some testimony about it. In any event, Elisha was not asked to return to the emergency by room by Dr. Handler for further evaluation after this telephone call.
Unaware that this telephone conversation had taken place between Dr. Handler and the second radiologist, Elisha returned home on November 17, 2015 with a call-back. She remained there until the next morning.
In the morning of November 18, 2015, Elisha’s condition became so bad that she had to be taken back to William Osler Health System – Brampton Civic Hospital by ambulance. She was referred for a surgical consultation during her time in the emergency room.
At approximately 5:00 p.m. on November 18, 2015, a general surgeon at the hospital completed his consultation and determined that an urgent laparoscopy needed to be performed. The surgeon also identified that a laparotomy might need to be performed. There were some issues on the timing of the surgery because Elisha needed to be stabilized before she could be operated on.
A laparoscopy is the insertion of a camera into the abdomen to determine whether there are issues. It is less invasive than a laparotomy, which is a full incision into the abdomen that allows for repairs to significant problems that exist in the abdomen, including problems with the small bowel.
The laparoscopy was performed at approximately 9:00 p.m. on November 18, 2015. The surgery revealed that Elisha’s bowel was herniated and showed signs of ischemia. Although the surgery had started out as a laparoscopy, a laparotomy was ultimately performed. The laparotomy resulted in the untwisting of Elisha’s bowels.
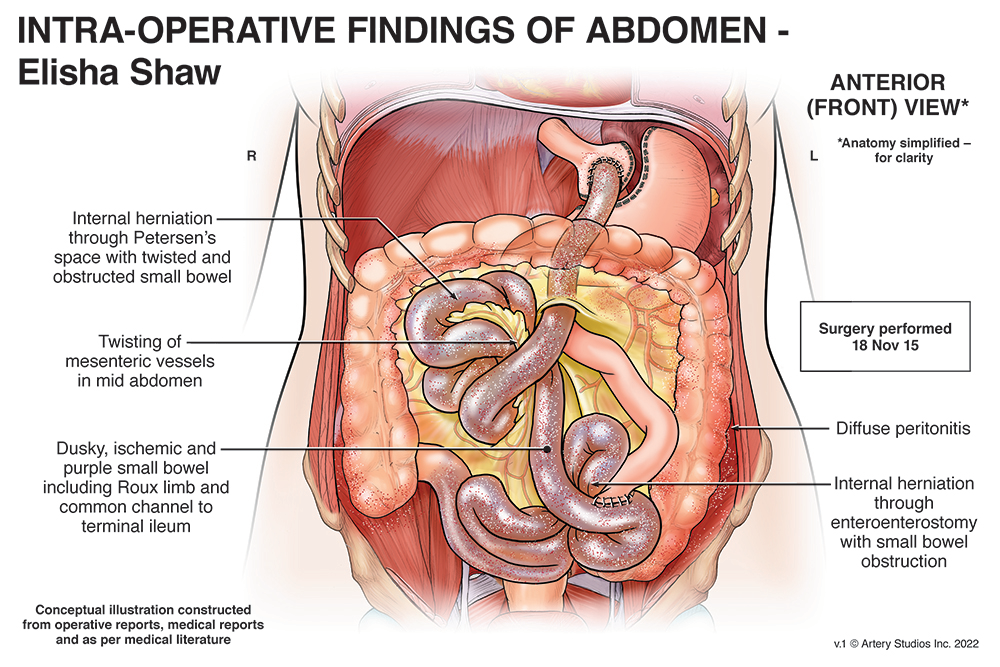
During this surgery, the surgeon consulted with the on-call bariatric surgeon at the Humber River Regional Hospital. After that consultation, the surgeon determined that the best course of action was to irrigate Elisha’s bowel and close the abdomen temporarily to give the small bowel time to see whether it would re-perfuse (regain its colour and blood circulation) or whether it was becoming necrotic and was going to have to be removed.
A further surgery was planned for twenty-four hours later to determine the status of Elisha’s small bowel.
Unfortunately, Elisha’s small bowel did not recover. In the morning of November 19, 2015, portions of Elisha’s small bowel were showing frank signs of necrosis. Therefore, a substantial resection of Elisha’s small bowel was performed.
Elisha’s prognosis was guarded and she was transferred to Humber River Regional Hospital. Elisha’s condition continued to deteriorate and further surgery was performed on November 22, 2015. This surgery resulted in the removal of other portions of her digestive system that had begun to show signs of necrosis.
This surgery was not successful. Elisha’s condition continued to deteriorate. She died on November 25, 2015 at the age of 34.
DECISION
Standard of Care
The trial judge succinctly found that Dr. Handler fell below the standard of care in his treatment of Elisha as follows [at para. 183]:
I conclude that Dr. Handler ought to have called Ms. Shaw back to the hospital and referred her to one of the surgeons on duty for an emergency consultation. Dr. Handler’s failure to do this was not a mere matter of judgment. Dr. Handler was mistaken in his view that Ms. Shaw’s symptoms had improved, and he had either missed or ignored the fact that Ms. Shaw’s pain was radiating into her back. Dr. Handler compounded these errors by brushing off the telephone call that he received from Dr. Fitzgerald outlining that Ms. Shaw had another one of the symptoms indicative of a hernia.
In coming to this conclusion, the trial judge referred to medical literature that existed at the material time that expressed the risks associated with a gastric bypass. None of the doctors disagreed with the the propositions set out in the literature, specifically that:
The trial judge further concluded that the potential long-term complications of gastric bypass surgery were well-known by emergency room doctors in Ontario. The defence emergency room physician and general surgeon tried to argue that these complications were not well-known at the time, however, the trial judge expressly rejected their evidence on this important point.
Causation
The trial judge concluded on the evidence that an earlier surgical consultation on November 17, 2015 (the day of Elisha’s first visit to the emergency room) would have led to a laparoscopic investigation that same day.
The result of that laparoscopic investigation would have been that the surgeon would have discovered, and repaired, the internal hernia that Elisha was suffering from.
If that had occurred, Elisha would not have died and would have been left with very little, if any, impairment from this incident at all. Moreover, the trial judge stated [at paras. 225-226]:
My reasons for reaching this conclusion are founded in the fact that, if the laparoscopic surgery had taken place on November 17th, 2015 instead of November 18th, 2015, the hernias would have been undone at a point when there was no necrosis in the bowels and the bowels would have still been healthy enough that necrosis would not have developed. Ms. Shaw’s condition would have been reversed by timely intervention and there would have been no need to resect any portion of her bowels.
As a result, I am of the view that, but for Dr. Handler’s negligence in not following up with Ms. Shaw, Ms. Shaw would not have died. Dr. Handler’ negligence caused Ms. Shaw’s death and, therefore, he is liable for the damages that flow from that negligence.
Damages
Elisha was a married mother of four children aged 7, 5, 4, and 2. She had loving relationship with her children and husband.

The damages awarded by the trial judge were as follows:
EXPERT LIABILITY WITNESSES
Plaintiffs’ Experts
Dr. Alan Drummond is an emergency medicine physician with extensive experience in the field. He was permitted to provide opinion evidence on the issue of the standard of care of an emergency physician in Ontario in 2015 regarding the management of a patient with abdominal pain.
Dr. Ron Holliday is a general surgeon and was qualified as a caustion expert. Dr. Holliday was noted to have extensive experience as a surgeon, both in performing surgery and in teaching at the University of Western Ontario. Dr. Holliday performed surgery at the Victoria Campus of the London Health Sciences Centre. He also taught in the Department of Surgery in the Schulich School of Medicine at UWO.
In his career as a surgeon, Dr. Holliday also had experience in both urgent abdominal and bariatric surgery, although Dr. Holliday did not perform in his practice the Roux-en-Y procedure that was performed on Elisha in 2012.
By the time of trial, Dr. Holliday continued to work one day a week at the Strathroy Hospital where he assists and mentors a young surgeon that works at that facility.
Defence Experts
Dr. Amit Shah is an emergency medicine physician and was qualified to give opinion evidence on the standard of care of an emergency physician practicing in Ontario in 2015
Dr. Timothy Jackson is a general and bariatric surgeon. He was qualified as a causation expert in general surgery and specifically in the involvement of a general surgeon in the care and treatment of a patient in the emergency room in 2015 and the impact of any delay in the treatment of Elisha’s abdominal pain in 2015.
Decision Date: September 6, 2023
Jurisdiction: Ontario Superior Court of Justice
Citation: Thompson v. Handler, 2023 ONSC 5042 (CanLII)
Ontario Superior Court finds Brampton doctor liable for negligence resulting in patient’s death.

A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

What College of Physicians and Surgeons of Ontario v. Thirlwell, 2026 ONPSDT 5 Means for Patients and Public Trust In College of Physicians and Surgeons