
Nurse Alters Morphine Record, Patient Dies: CNO Orders Permanent Resignation
A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

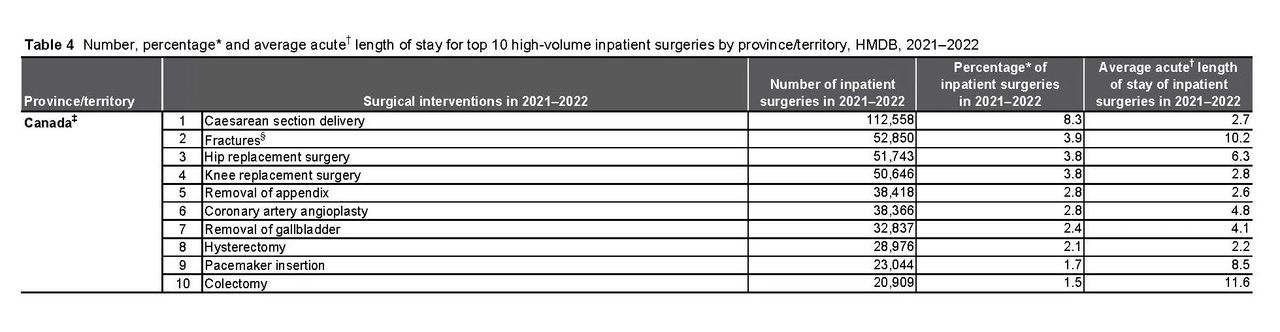
According to the Canadian Institute for Health Information (CIHI), there are approximately 200,000 surgical procedures performed every month in Canada. This number has been affected by the COVID-19 global pandemic with a pre-pandemic monthly surgical average of 231,000 per month versus a post-pandemic surgical average of 192,000 per month. The CIHI data table showing pre- and post-pandemic surgical data is available here.
With approximately 2.4 million surgical procedures performed in Canada every year, there will unfortunately be some occurrences of surgical negligence. However, not all bad surgical outcomes are the result of negligent or substandard care. Surgical procedures carry certain recognized risks that may occur even with appropriate medical care. The reality is that not every patient comes out of surgery perfectly healthy.
For this reason, surgical negligence claims are among the most challenging of all medical malpractice claims to prove in court. For many surgical procedures, the patient is under general anesthesia and therefore will have no knowledge of the procedure itself. The operative report, which is often (though not always) considered the best evidence of the procedure is dictated by the surgeon. Therefore, patients who find themselves waking up with serious complications may find it difficult to prove that their bad surgical outcome was caused by negligent medical care.
In this post, I will explain in detail how an experienced medical malpractice lawyer will investigate and analyze a potential surgical malpractice claim to determine whether you may have a claim for financial compensation due to the negligence a physician, hospital and/or nurse.
THE MAIN AREAS OF INVESTIGATION INTO A SURGICAL NEGLIGENCE CLAIM
When a patient (or their family) first consults with a lawyer, they are often understandably focused on the fact that they had a bad outcome from a surgery which has resulted in substantial morbidity or mortality. They may not have a clear understanding of where or how things went wrong. Without reviewing all of the medical records, a medical malpractice lawyer will not know either.
For this reason, your lawyer will want to examine not only the surgery itself, but all the potential areas where there could be legal liability for a surgical error, which includes pre- and post-operative care, in addition to the intra-operative care.

Pre-operative care is everything that happened before your surgery. This area of investigation would focus on whether the patient was a good candidate for the procedure in the first place. It can sometimes be the case that a surgeon inappropriately recommends a particular type of surgery. This can become complicated if pre-operative investigations, such as radiological imaging, were erroneously interpreted causing a cascading effect of errors.
A potential delayed diagnosis would also fall into the pre-operative care analysis. In some cases, earlier surgical intervention leads to better outcomes. For example, it is usually easier to remove a tumor when it is smaller and more confined to a particular area of the body versus when it is larger and has infiltrated into other areas.
Another important area of analysis with respect to potential negligent pre-operative care is with respect to informed consent. The law of informed consent requires a patient to be told of the material risks and benefits of a potential surgical procedure, as well as potential alternatives to surgery. If they are not made aware of the materials risks and benefits, they cannot have given legal consent to the procedure. To succeed, it will also be necessary to prove not only that the patient would have declined the procedure if properly informed, but that any reasonable person in the same situation would have as well.

Intra-operative care relates to the surgery itself. In this area of investigation there are a number of important considerations. Most often the concern is that something unexpected happen during the surgery. At the most extreme end, the patient died during or immediately after the surgical procedure was completed. In other cases, there is an unexpected outcome such as damage to adjoining vessels or organs. A medication error with respect to the anesthesia could occur causing severe hypotension or some other adverse effect. In other cases, a surgical instrument may have been inadvertently left behind inside the patient. It can also sometimes happen that a surgeon may accidently operate on the wrong part of the body or wrong limb.
Proving intra-operative negligent care is challenging since the main evidence regarding how the surgery was performed will come from the surgeon. All surgical procedures are documented. Most often the details of the procedure are dictated into an operative report that will become part of the patient’s health record. In addition to the operative report, there will often be an anesthesia record as well as an operative record that contains information about the hospital resources and perioperative nurses involved. It is not uncommon that a patient experiences a serious complication yet the medical records reflect a completely normal procedure. This scenario will require analysis into whether such an outcome could occur without negligence.
Complications can certainly occur for which the surgeon should not be faulted. There are risks of surgery and bad outcomes can and do happen. This where analyzing the surgical approach and technique becomes important. If the surgeon failed to follow standard surgical technique and a complication occurs then there will probably be a strong case for surgical malpractice. If the surgeon can establish that standard procedure was followed then they may not be faulted despite the complication occurring.

Post-operative care is your management after the surgery. The main area of concern in post-operative care is failing to identify a surgical complication in a timely manner which then results in significant disability or even death. For instance, a patient may start developing sepsis after abdominal surgery if their bowel was injured. If this post-operative complication is recognized and treated early, the patient should do well. If, however, it goes unrecognized for too long, the patient may pass the point of no return and die.
Post-operative care is often the responsibility of the surgeon, particularly while the patient is in hospital. Nurses are often implicated in substandard post-operative care cases when worrisome signs and symptoms are not properly communicated to a physician resulting in delayed care.
Some post-operative complications can take more than a few days or weeks to present which can be after the patient has been discharged from hospital. This can result in the patient presenting themselves to the emergency room where a misdiagnosis or delayed diagnosis may occur resulting in a bad outcome. For these reasons, when analyzing the appropriateness of post-operative care, all aspects of the patient’s post-operative course must be reviewed.
Surgical negligence claims are challenging to prove in court, but the focus should not be exclusively on the procedure itself. When a patient unfortunately suffers significant harm from a surgery, a medical malpractice lawyer will need to review all aspects of the care, including the pre- and post-operative care in addition to the actual surgery.
MOST FREQUENT SURGERIES IN CANADA AND POTENTIAL MEDICAL-LEGAL CONCERNS
The CIHI has data on the total number of different types of surgeries performed in Canada in the years 2021-2022. By the far, the most frequent surgery in Canada is the Caesarean section delivery with 112,558 of these performed during this time. This is followed by fracture surgeries, hip replacement, knee replacement, appendix removal, coronary angioplasty, removal of gallbladder, hysterectomy, pacemaker insertion and colectomy surgeries.
Medical-legal concerns can arise from any surgical procedure and are generally set out above. Each surgical procedure will have specific areas of concern, some of which will be reviewed below.
Caesarean section delivery (“C-section”) is the most frequent surgery in Canada. It makes up 8.3% of all inpatient surgeries. The most concerning potential complication from a C-section would be a birth injury. This could arise because an expectant mother was not taken to a C-section earlier when indicated, potentially because of fetal distress or another medical reason. Due to the delay in delivering the baby, the baby may have died or suffered a serious brain injury resulting in cerebral palsy and associated life-long disability.
Fractures are the next most frequent type of surgery performed. This would include fracture surgeries for a very wide variety of fractures. There are 206 bones in the human body and so you can imagine all the different types of fracture surgeries that could be performed. That being said, the most common type of medical-legal concerns arising from fracture surgeries would be related to the timing of the surgery itself, poor surgical technique resulting in poor healing and revision surgery, and in extreme cases, amputations or death.
Removal of appendix (appendectomy), gallbladder (cholecystectomy), uterus (hysterectomy) and colon (colectomy) are all frequent surgeries as noted in the table above. These surgeries would fall into the realm of pelvic and abdominal surgeries which carry medical-legal concerns for bleeding, infection, and injury to adjourning anatomical structures. The effect of some of these complications can be devastating in some cases.
HOW DO I PROVE A SURGICAL NEGLGIENCE CLAIM?
Proving any kind of medical malpractice claim in Ontario is challenging. For more information on whether you can sue for medical malpractice, please read this post.
In order to prove surgical negligence, you will need an expert opinion from a qualified and experienced surgeon with similar training and background as the surgeon in question. So much will depend on the specific areas of concern with respect to the surgical care which is why consulting with a lawyer is essential to understanding your legal rights.
If you are concerned that you or a loved one has been harmed as a result of a surgical error, you should seek legal advice from an experienced medical malpractice lawyer to learn whether you may be entitled to compensation.

A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

What College of Physicians and Surgeons of Ontario v. Thirlwell, 2026 ONPSDT 5 Means for Patients and Public Trust In College of Physicians and Surgeons