
Nurse Alters Morphine Record, Patient Dies: CNO Orders Permanent Resignation
A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

Most people going to the emergency room are genuinely concerned that they have something seriously wrong with them. After being assessed by an emergency physician, they are often relieved to learn that they are not suffering from anything life-threatening or serious.
Fortunately, the vast majority of emergency visits end up being for relatively benign medical concerns. However, sometimes patients present with serious medical conditions that require prompt diagnosis and intervention to save their life or limb. These rare cases require careful identification by emergency physicians and nurses who are trained to consider and rule out life threatening conditions at an early stage. Unfortunately, sometimes diagnoses are missed in the emergency room and patient care is delayed with devastating consequences.
Here is a list of the top 5 most dangerous medical conditions to be misdiagnosed with in the emergency room.
1. Ruptured Brain Aneurysm
A cerebral or brain aneurysm is a bulge or ballooning in a blood vessel in the brain. An aneurysm often looks like a berry hanging on a stem.
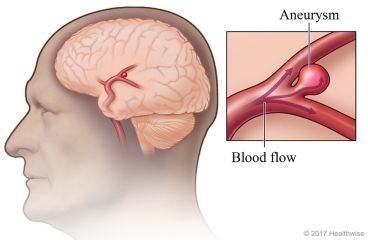
A brain aneurysm can leak or rupture, causing bleeding into the brain (hemorrhagic stroke). Most often, a ruptured brain aneurysm occurs in the space between the brain and the thin tissues covering the brain. This type of hemorrhagic stroke is called a subarachnoid hemorrhage.
A ruptured aneurysm quickly becomes life-threatening and requires prompt medical treatment.
In a 2023 medical journal article entitled “Duration between aneurysm rupture and treatment and its association with outcome in aneurysmal subarachnoid haemorrhage“, the authors warn that timely treatment of aneurysmal subarachnoid hemorrhage is key to prevent further rupture and poor outcome.
Early treatment (first 24–48 h) can prevent rebleeding and consecutively reduce likelihood for poor functional outcome. Several factors influence treatment delay, most importantly delay in hospital admission and delay in treatment. Delay in hospital admission is most frequently caused by the need to transfer a patient from another hospital. This can be due to initial misdiagnosis, reported to be as high as 51%. Delay in correct diagnosis has markedly decreased as shown in previous studies.
A delay in diagnosis and treatment of a ruptured brain aneurysm beyond the first 24 hours is associated with a higher mortality rate.
2. Heart Attack (Myocardial Infarction)
A heart attack occurs when the flow of blood to the heart is severely reduced or blocked. The blockage is usually due to a buildup of fat, cholesterol and other substances in the heart (coronary) arteries. The fatty, cholesterol-containing deposits are called plaques. The process of plaque buildup is called atherosclerosis.
Sometimes, the plaque can rupture and form a clot that blocks blood flow. A lack of blood flow can damage or destroy part of the heart muscle.
Signs and symptoms of heart attack include:
Early diagnosis and treatment of myocardial infarction can prevent life-threatening complications such as dysrhythmias and death.
In a 2021 medical journal article entitled “Misdiagnosis of Acute Myocardial Infarction: A Systematic Review of the Literature” the authors found that the common initial misdiagnoses that subsequently had [acute myocardial infarction] were ischemic heart disease, nonspecific chest pain, gastrointestinal disease, musculoskeletal pain, and arrhythmias. Reasons for missed [acute myocardial infarction] include incorrect electrocardiogram interpretation and failure to order appropriate diagnostic tests. Hospitals in rural areas and those with a low proportion of classical chest pain patients that turned out to have [acute myocardial infarction] were at greater risk of missed [acute myocardial infarction].
Women are more likely to be misdiagnosed with a heart attack over men. In a post dated February 28, 2022 by Columbia University Irving Medical Center it is observed that identification and treatment of myocardial infraction for women is regularly delayed and often misdiagnosed.
Women are more likely to have an atypical presentation including symptoms such as shortness of breath, nausea, and fatigue. Coupled with guidelines created for men, this can lead to a missed diagnosis in women, or a misdiagnosis, with women’s heart disease often categorized as gastrointestinal problems or anxiety.
3. Stroke
A stroke happens when blood stops flowing to any part of your brain causing damage to brain cells.
Stroke is the leading cause of long term disability in developed countries and one of the top causes of mortality worldwide.
There are three main types of stroke: ischemic stroke, hemorrhagic stroke, and transient ischemic attack (TIA).
An ischemic stroke is caused by a blockage or clot in a blood vessel in your brain. The blockage can be caused when plaque builds up on the inside wall of an artery.
Ischemic strokes are further divided into 2 groups: thrombotic strokes which are caused by a blood clot that develops in the blood vessels inside the brain and embolic strokes that are caused by a blood clot or plaque debris that develops elsewhere in the body and then travels to one of the blood vessels in the brain through the bloodstream.
About 87% of all strokes are ischemic.
A hemorrhagic stroke occurs when an artery in the brain breaks open. The interrupted blood flow causes damage to your brain. High blood pressure weakens arteries over time and is a major cause of hemorrhagic stroke
A TIA is when a small clot briefly blocks an artery. This is sometimes called a mini-stroke or warning stroke. The TIA symptoms usually last less than an hour, and may only last a few minutes. TIAs are an important warning that a more serious stroke may occur soon.

In the Canadian Stroke Best Practice Recommendations, Acute Stroke Management 7th Edition, Update 2022, published by the Heart and Stroke Foundation of Canada, the authors state:
Acute stroke is a medical emergency and optimizing out-of-hospital (prehospital) care improves patient outcomes. EMS plays a critical role in prehospital assessment and management of patients with suspected stroke. Acute interventions such as thrombolytic therapy and EVT are time sensitive; therefore, strategies to reduce delays such as re-directing ambulances to stroke centres and prenotification by EMS staff can help identify patients with more severe strokes who may be eligible for such treatments.
Intravenous thrombolytic therapy should be administered within a 4.5-hour treatment window, while EVT is best performed within 6 hours from stroke onset. In selected patients, EVT can be used in combination with intravenous thrombolysis (given within 4.5 hours of symptom onset), with numbers needed to treat reported as low as 3 – 4. EVT is also beneficial as a sole treatment for those persons who are ineligible for intravenous thrombolysis. In addition, a small group of patients may still benefit from EVT up to 24 hours from symptom onset when selected by neurovascular imaging in the context of a coordinated stroke system that includes access to experts in stroke and neurointerventional care.
A delayed or misdiagnosis of stroke could result in a patient not receiving critical interventions at an early stage before significant brain damage occurs.
4. Cauda Equina Syndrome
The collection of nerves at the end of the spinal cord is known as the cauda equina, due to its resemblance to a horse’s tail. The spinal cord ends at the upper portion of the lumbar (lower back) spine. The individual nerve roots at the end of the spinal cord that provide motor and sensory function to the legs and the bladder continue along in the spinal canal.
The cauda equina is the continuation of these nerve roots in the lumbar and sacral region. These nerves send and receive messages to and from the lower limbs and pelvic organs.

Cauda equina syndrome (CES) occurs when there is dysfunction of multiple lumbar and sacral nerve roots of the cauda equina.
According to the American Association of Neurological Surgeon, patients with CES may experience some or all of these “red flag” symptoms.
Early diagnosis and treatment is key to preventing significant disability. According to the American Academy of Orthopedic Surgeons:
If patients with cauda equina syndrome do not receive immediate, appropriate treatment to relieve the pressure, it can result in permanent paralysis, impaired bladder and/or bowel control, loss of sexual sensation, and other problems. Even with immediate treatment, some patients may not recover complete function; earlier treatment does, however, offer the best outcomes for cauda equina syndrome.
5. Compartment Syndrome
Compartment syndrome occurs when pressure rises in and around muscles. The pressure is painful and can be dangerous. Compartment syndrome can limit the flow of blood, oxygen and nutrients to muscles and nerves. It can cause serious damage and possible death.
Compartment syndrome occurs most often in the lower leg. But it can also impact other parts of the leg, as well as the feet, arms, hands, abdomen (belly) and buttocks.
There are two kinds of compartment syndrome:
Prompt diagnosis and treatment is imperative to avoid a catastrophic outcome.
In a 2022 medical journal entitled “Acute Compartment Syndrome“, the authors noted that the prognosis after treatment of compartment syndrome depends mainly on how quickly the condition is diagnosed and treated. When fasciotomy is done within 6 hours, there is almost 100% recovery of limb function. After 6 hours, there may be residual nerve damage. Data show that when the fasciotomy is done within 12 hours, only two-thirds of patients have normal limb function. In very delayed cases, the limb may require an amputation.

A Profound Breach of Trust in End-of-Life Care In CNO v. Lindsey Coyle, the Discipline Committee of the College of Nurses of Ontario addressed one

What College of Physicians and Surgeons of Ontario v. Thirlwell, 2026 ONPSDT 5 Means for Patients and Public Trust In College of Physicians and Surgeons